Introduction: Magnetic Resonance Imaging (MRI) is a powerful medical imaging technique that provides detailed images of the body’s internal structures, allowing healthcare professionals to diagnose and monitor a wide range of medical conditions. Interpreting MRI scans requires specialized knowledge and expertise to accurately identify abnormalities, assess disease progression, and guide treatment decisions. In this comprehensive guide, we delve into the intricacies of MRI interpretation, exploring the principles, techniques, and considerations involved in analyzing MRI images for clinical diagnosis and management.
- Principles of MRI Imaging: MRI imaging relies on the principles of nuclear magnetic resonance (NMR) to generate high-resolution images of anatomical structures and physiological processes within the body. When placed in a strong magnetic field and exposed to radiofrequency pulses, hydrogen nuclei in water molecules align with the magnetic field and emit radiofrequency signals, which are detected by sensitive receivers and converted into images. Different tissues exhibit unique magnetic resonance properties, such as relaxation times and proton densities, which contribute to image contrast and tissue differentiation in MRI scans.
- Image Acquisition Techniques: MRI scanners utilize various imaging sequences and pulse sequences to capture different types of information about tissue composition, structure, and function. Common MRI sequences include T1-weighted imaging, T2-weighted imaging, proton density imaging, and diffusion-weighted imaging (DWI), each of which highlights specific tissue characteristics and pathological features. Advanced MRI techniques such as magnetic resonance angiography (MRA), magnetic resonance spectroscopy (MRS), and functional MRI (fMRI) provide additional insights into vascular anatomy, tissue metabolism, and brain function, respectively.
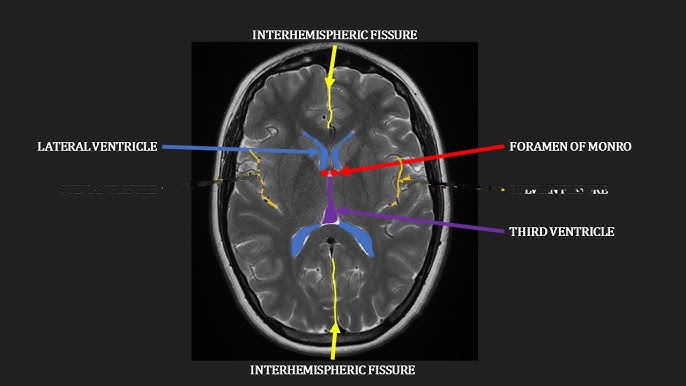
- Anatomical Landmarks and Normal Variants: Interpreting MRI scans requires a thorough understanding of anatomical landmarks and normal variants across different body regions. Radiologists and clinicians must be able to identify and differentiate normal anatomical structures, such as organs, blood vessels, nerves, and bones, from pathological findings. Knowledge of normal variants, such as anatomical variations, developmental anomalies, and incidental findings, is essential for distinguishing benign conditions from potential pathology and avoiding misinterpretation or unnecessary interventions.
- Recognizing Pathological Findings: MRI scans may reveal a wide range of pathological findings, including tumors, inflammation, infection, trauma, degeneration, and vascular abnormalities. Radiologists and clinicians must carefully evaluate MRI images for signs of abnormal tissue signal intensity, morphology, and enhancement patterns that may indicate underlying pathology. Common imaging features of pathology include mass effect, edema, necrosis, hemorrhage, enhancement, and diffusion restriction, which can vary depending on the nature and location of the underlying disease process.
- Differential Diagnosis and Pattern Recognition: Interpreting MRI scans often involves generating a comprehensive list of differential diagnoses based on the imaging findings and clinical context. Radiologists and clinicians rely on pattern recognition and diagnostic algorithms to systematically evaluate MRI images and prioritize potential etiologies for further investigation. Comparative analysis with previous imaging studies, laboratory tests, and clinical history is crucial for refining the differential diagnosis and guiding subsequent diagnostic workup and management.
- Quantitative Analysis and Image Post-processing: In addition to qualitative assessment, MRI interpretation may involve quantitative analysis and image post-processing techniques to extract numerical data and derive quantitative biomarkers of disease severity and treatment response. Quantitative MRI techniques, such as volumetric analysis, diffusion tensor imaging (DTI), and functional connectivity analysis, provide objective measures of tissue morphology, microstructure, and functional connectivity, which can aid in disease characterization and monitoring over time.
- Pitfalls and Artifacts: MRI interpretation is susceptible to various pitfalls and artifacts that can mimic or obscure pathological findings, leading to diagnostic errors or misinterpretation. Common MRI artifacts include motion artifacts, susceptibility artifacts, chemical shift artifacts, aliasing artifacts, and flow-related artifacts, which can arise from patient motion, magnetic field inhomogeneities, hardware imperfections, and physiological motion. Radiologists and clinicians must be aware of these artifacts and employ corrective measures to minimize their impact on image quality and diagnostic accuracy.
- Clinical Correlation and Multimodal Imaging: Effective MRI interpretation requires close collaboration between radiologists, clinicians, and other healthcare providers to integrate imaging findings with clinical data and laboratory results. Multimodal imaging approaches, such as combining MRI with computed tomography (CT), positron emission tomography (PET), ultrasound, or nuclear medicine imaging, offer complementary information and enhance diagnostic accuracy for complex cases. Clinical correlation and multidisciplinary discussions are essential for reaching consensus on diagnosis, treatment planning, and patient management.
Conclusion: Interpreting MRI scans is a complex and multidimensional process that requires a deep understanding of imaging principles, anatomical structures, pathological findings, and clinical correlations. By mastering the art of MRI interpretation, healthcare professionals can provide accurate diagnoses, personalized treatment plans, and optimal patient care across a wide range of medical specialties and clinical settings. Through continuous education, collaboration, and technological innovation, MRI imaging remains a cornerstone of modern medicine, driving advances in diagnosis, therapy, and patient outcomes.